Fine Needle Aspiration
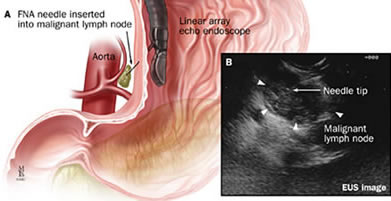
EUS-guided fine-needle aspiration (FNA) is performed in many large medical centers as part of routine esophageal cancer staging. The main clinical utility of EUS-FNA is cytological diagnosis of regional and distant tumor metastasis, which can diagnose tumor stage and influence treatment decisions.
The goal of FNA is to obtain cytological evidence of cancer (or confirm non presence of cancer cells) through tissue or fluid acquisition to diagnose and stage the extent of GI diseases. A fundamental principle of EUS-FNA is that the information obtained should have the potential to affect patient management. In addition, the indications for EUS-FNA should be guided by its diagnostic accuracy, cost effectiveness, patient comfort and safety. Using a linear scope which has a working channel, needles can be used to shrink cysts, sample tumors and take biopsies.
Contraindications/Challenges of FNA
EUS-FNA can acquire the diagnostic cells and tissue sample by puncturing a target organ through the digestive tract wall. Contraindications for EUS-FNA include “situations in which the FNA result would not affect management, inability to clearly visualize a lesion, a tumor mass or vessel interposed between the needle-to-target path, bleeding diathesis and risk of tumor seeding.” However, the advantages of doing an EUS/FNA is that it:
- Aids in the assistance in the staging and tissue acquisition of malignant disease through the EUS-guided FNA
- Aids in the assessment of benign disease
- Aids with interventional applications such as celiac plexus block or neurolysis and pseudocyst drainage
Specimen Handling of FNA
When solid tissue is sampled, a small amount of material accumulates in the hub of the needle. This material is immediately and gently expelled onto a clean glass slide, spread in a thin layer and rapidly dried by waving the slide in the air or by placing it in front of a fan or portable hair dryer. This is called making an “air-dried smear.” The slide is then stained with special dyes and examined under the microscope.
When a fluid sample is collected, air-dried smears are often prepared directly from the material in the syringe, and the remaining fluid is placed in transport tubes or containers. The smears and the containers are then sent to the laboratory for further analysis. This typically includes measurement of the cellularity and protein content of the fluid, as well as preparation of additional slides. If the sample is very thin and watery, sometimes the sample is concentrated before the slides are made, which provides more cells to look at. The slides are then stained with special dyes and examined for carcinoembryonic antigen (CEA), amylase levels and cytology.